
Goodbye MU, Hello PI: A new focus on patient-centered interoperability

In April 2018, The Centers for Medicare and Medicaid Services (CMS) announced that the previous EHR incentive program commonly known as “Meaningful Use” (MU) will be renamed and adapted into a program called “Promoting Interoperability” (PI). This rebranding reflects the importance that CMS has placed on electronic interoperability in healthcare. The final rule, released by CMS on August 2, highlighted a change in measures and scoring methodology to increase the importance of patient electronic access to health information.
Under the old Meaningful Use program, the measures were considered pass/fail on a threshold basis, requiring hospitals to meet certain thresholds to receive credit for completing a measure. Under the new proposed rule, measures would be given a point score based on a performance ratio, meaning if the hospital performed a measure 50% of the time, they would receive 50% of that measure’s allotted points. To be considered a meaningful user, a hospital must achieve 50 of 100 possible points.
The points are weighted to reflect a clear emphasis on providing patients electronic access to their health information, account for 40 of the 100 points a hospital is able to earn in 2019. CMS has stated that this measure is the crux of the PI program and the exchange of data between provider and patient is imperative in order to achieve interoperability, and thus improve health outcomes. This flow of data creates patient-centered interoperability, as the patient acts as the hub for all their health data.
The Possible Future for PI Scoring
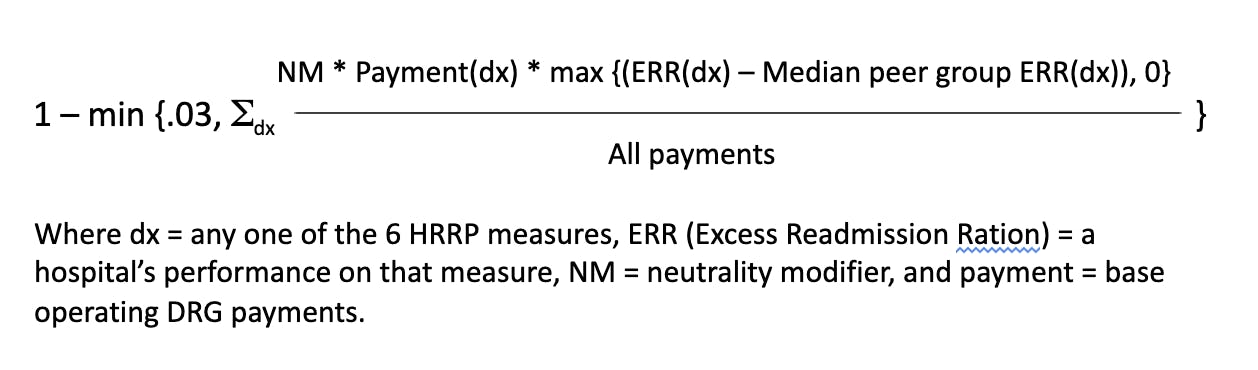
In analyzing the shift from fee-for-service to value-based purchasing in Medicare, and looking at similar performance-based payment incentive programs, such as the Hospital Readmissions Reduction Program (HRRP) and the Hospital-Acquired Conditions Reduction Program (HACRP), it can be inferred that one’s performance score for PI may become more and more crucial. Currently, the scoring methodology for payment adjustments incurred in the Hospital Readmissions Reduction Program and the Hospital-Acquired Conditions Reduction Program is based on a comparison of how well a hospital performs against the performance of other hospitals. Both programs use complex mathematical formulas to determine a hospital’s score, and therefore applicable payment reduction.
The 21st Century Cures Act of 2016 mandated a new stratified scoring methodology for the Hospital Readmissions Reduction Program that evaluates hospital performance relative to other hospitals with similar proportions of patients. Under this program, hospital payments can be reduced by a maximum of 3%.
The payment adjustment factor for the HRRP is calculated thusly:
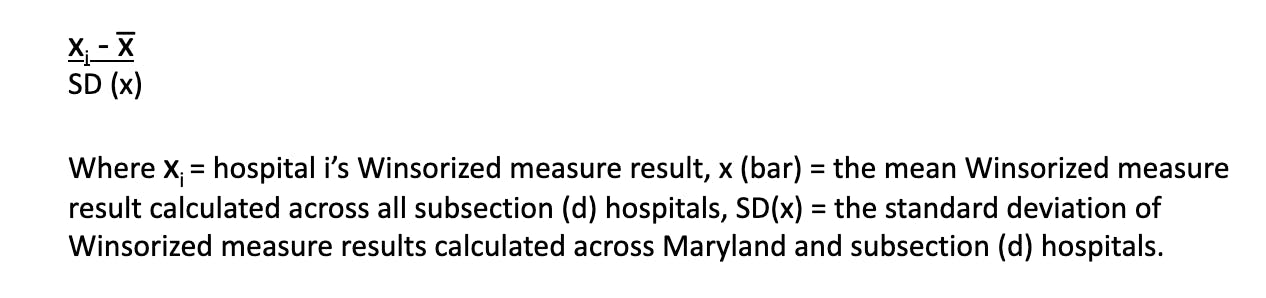
The Hospital-Acquired Conditions Reduction Program uses a Winsorized z-score methodology that ranks hospitals on a continuous spectrum from best performing to worst performing. Hospitals that rank in the bottom 25% of that spectrum will be subject to a 1% payment reduction.
The Windsorized z-score formula for “Hospital i” is:
These complexly calculated, comparison-based methodologies set forth by other payment incentives/penalty quality initiative programs, coupled with the fact that CMS has in the past restructured scoring methodologies as their priorities changed, lead us to infer that in the future, CMS could follow a similar approach for the PI program and adopt similar, more complexly scored comparison-based payment penalties.
The Penalties
The payment adjustments for PI are in keeping with the structure that was established for MU. No changes have been made in the penalties incurred for not being a meaningful EHR user. As was in 2017 and 2018, the penalty for 2019 and beyond will be 75% of the percentage increase to the Inpatient Prospective Payment System (IPPS). For example, if the increase to IPPS for a given year was 2%, a hospital that does not participate or does not meet Promoting Interoperability would only receive a 0.5% increase.
For 2019, the Final Rule has set forth a total update percentage of 1.85% for Medicare inpatient services, making the PI penalty for 2019 1.38% (75% of 1.85).
In 2017, inpatient payments to hospitals neared $300 billion (CMS Trustees Report 2018). Using that figure as an estimate, hospitals are collectively at risk for losing approximately $4 billion for not meeting Promoting Interoperability.
The Technology
The IPPS Final Rule requires that for the 2019 reporting year, hospitals must be using the 2015 Edition certification criteria for their certified EHR technology (CEHRT). This requirement is in alignment with what was expected for Meaningful Use Stage 3. According to the Office of the National Coordinator for Health IT, as of June 2018, 90% of hospitals have the 2015 Edition certified technology available from their EHR vendors.
The Measures
For Promoting Interoperability measures, CMS has stated a desire to reduce administrative burden, provide flexibility and streamline the providers’ workflow. The overall number of required measures has been reduced from 16 to 6. CMS Administrator Seema Verma said they are removing measures that the majority of providers are performing well on, duplicative measures, and measures that are excessively burdensome to report. Some measures have been modified, combined, and renamed, with the goal of putting the focus of the program on health data exchange and interoperability.
Two new measures have been adopted to address the rising opioid crisis. For 2019 and 2020 CMS has finalized the measure Verify Opioid Treatment Agreement as an optional measure with the ability to earn 5 bonus points each year. The measure Query of Prescription Drug Monitoring Program will be an optional measure in 2019 worth up to 5 bonus points and becomes a requirement in 2020, worth up to 5 points.
Table: The Streamlining of Measures from MU to PI
Summary of Removed and Final Measures Beginning with the EHR Reporting Period in CY 2019
The Scoring
CMS has finalized a new scoring methodology for the Promoting Interoperability program. Under the old Meaningful Use scoring methodology, measures were given a “pass/fail” once a certain threshold was attained. The new methodology gives hospitals a performance-based score for each measure they are required to report. For example, performing a measure on 50% of all patients discharged within the 90-day reporting period will result in achieving 50% of the earnable points. The scores are weighted to reflect the priority of the measures, so that hospitals attain more points for prioritized measures. The point scores of the individual measures are added together to calculate the total PI score. A total score of 50 points or more is required to satisfy Promoting Interoperability, and thus avoid a Medicare payment reduction. Eligible hospitals must report on all required measures in order to earn any score at all. Failure to report on any of the required measures (unless an exclusion applies), or reporting a “no” on a yes/no measure would result in a PI score of zero.
CMS believes that the introduction of a performance-based scoring methodology will allow them to shift the emphasis from merely being a meaningful user of EHR technology to achieving interoperable, patient-centered care.
Table: Example of Scoring
Patient Access
As the measure “Provide Patients Electronic Access to Their Health Information” has been weighted the most heavily, it is now exceedingly critical that hospitals strive to meet this measure for all of their discharged patients. In order to satisfy the measure, hospitals must:
1. Provide patients timely access (within 36 hours of its availability to the hospital) to view, download and transmit their health information and
2. Ensure that patient health information is available for the patient to access using any third-party application of their choice that is configured to meet the technical specifications of the application programming interfaces (API).
CMS defines “providing access” as supplying patients with all of the necessary information needed to view, download or transmit their information. This includes providing patients instructions on how to access their health information, a website address they can visit for online access, a unique, registered username and password, instructions on how to create a login, or any other instructions, tools or materials that patients need in order to view, download or transmit their information.
The Importance of APIs
In the proposed rule for Promoting Interoperability, CMS has highlighted the importance of APIs, stating, “API functionality supports health care providers and patient electronic access to health information. These functions allow for patient data to move between systems and assist patients with making key decisions about their health care. … Furthermore, the API allows for third-party application usage with more flexibility and smoother workflow from various systems than what is often found in many current patient portals.” (CMS-1694-P, 1335-6)
The Provider to Patient Exchange objective promotes patient awareness and involvement in their health care through the use of APIs and ensures patients have access to their medical data.
For the first time, hospitals will be required to use CEHRT that provides API functionality, and ensure that said functionality is fully enabled to allow patients to access their health information using a third-party application. A hospital may not block access to information or prohibit patients from using any application leveraging the API that meets the technical and security requirements.
The measure guidance from CMS states “Eligible hospitals are expected to provide patients with detailed instructions on how to authenticate their access through the API and provide the patient with supplemental information on available applications that leverage the API.”
If a patient elects to “opt-out” of participation in the measure, the hospital may still count the patient in the numerator, if the patient is provided all the necessary information to access their health data at a later time, i.e. opt back in without further follow-up action by the hospital.
How Can I Satisfy the API Requirement?
OneRecord offers a solution to providers seeking to meet the API requirement of the Providing Patient Access measure. We offer a patient-facing that allows users to access and aggregate their medical records across multiple providers’ EHRs, leveraging APIs.


